State Farm v. 654987
In State Farm v. 654987 filed in 2011, State Farm claimed there was a group of surgeons who were performing percutaneous discectomies on patients that did not need them in order to get big settlements on injury cases. State Farm also claimed that a large personal injury firm was closely tied to this because their brother and cousin were affiliated with company that supplied the “Spine Wand” device to the surgeon. According to State Farm, roughly 1,550 patients received percutaneous lumbar discectomies in Florida during 2005 to 2008 and almost 30% of those were done at the same surgery center in Palm Beach County Florida.
Discograms: Before performing the PD, one doctor, an anesthesiologist, would perform a discogram and reported that some form of pathology in one of the patient’s discs is a cause of the pain and that the patient would benefit from a PD.
A legitimate discogram is a diagnostic procedure that can be used to identify discs that are causing pain, however, there is a high chance of false positives. If a doctor suspects that a patient’s pain may be caused by pathology inside a disc, the doctor performing the discogram will inject dye into the disc and monitor the pressure building in the disc in pounds per square inch (“psi”). If the patient reports pain during pressurization of the disc, that particular disc is considered positive as a possible source of pain. If the patient doesn’t report any pain during pressurization of the disc, then that particular disc is considered negative and is likely not the source of the pain. The International Spine Intervention Society acknowledges that discograms are easily subject to abuse and created protocols including: (a) selecting patients who would not be prone to over-reporting pain; (b) performing a discogram on a healthy disc immediately above or below a “bad” disc to confirm a negative finding for pain; (c) scoring positive responses at more or less than 6 on a scale of 1-10 with pressurization of a disc at 50 psi or less; (d) validating the patient’s initial pain response by recording the persistence of pain at 30-60 seconds post provocation; (e) repeating pressurization of the disc to see if the patient reports the same/similar level of pain; and (f) if pain is reported upon injection of a disc, it should be confirmed by injecting a numbing agent to see if it eliminates the pain.
In this case, the anesthesiologist did not score the pain responses on a scale of 1-10 for any patient, did not document whether any patient’s pain persisted for 30-60 second after the injection and pressurization, did not repeat the pressurization in any positive disc to see if the patient reported the same pain, and did not inject any numbing agent into the positive disc to determine if it would eliminate the patient’s pain. Virtually every patient who received a discogram from this anesthesiologist was recommended for a PD.
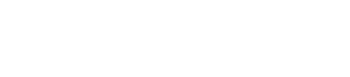
Percutaneous Discectomy: The Spine Wand is a long probe that is inserted into the nucleus of a disc. Radio frequency waves are then emitted from the tip of the probe to dissolve a small amount of tissue from the nucleus, and thermal energy is used to stabilize the remaining disc material. The Spine Wand is then withdrawn from the disc. In theory, this procedure decompresses the disc which, in turn, removes unwanted pressure that a contained protrusion is having on nerve roots. On September 29, 2008, Medicare issued a national noncoverage determination for a variety of thermal intradiscal procedures, including PDs.
Allegation of CPT Upcoding: In 2002, the company that manufactured the Spine Wand asked the AMA for a written letter regarding which was the correct CPT and was informed that 62287 was correct. Prior to 2006, the doctors mentioned in this lawsuit billed 62287 for the PD procedure. State Farm agreed was the correct code but stated that the procedures were unnecessary.
In August 2006, all of the doctors mentioned in this lawsuit began billing 63056 and 63057 which is an “open” discectomy and a more invasive procedure than what was actually performed. This is likely because if they performed an “incision” they were able to bill more whereas, if they continued performing the PD’s the way they had for years- with no incision, they would be reimbursed less. As you can see below, it is intentionally very thin so that no incision should be necessary:
In February 2009, the company that manufactured the Spine Wand conducted an internal audit which reported that they recommended and advocated medical providers to use a CPT code that was not approved by the AMA and “may not have properly described the procedure” that was performed.
DISCLAIMER
This is based on a real court case that was previously filed against a medical provider/doctor. The case number has been partially redacted and names have been changed to protect the Defendants’ names. This example is posted to help educate others on the laws and potential pitfalls. This posting is not intended to embarrass or defame anyone. I have limited the information and simplified some of the facts in the lawsuit to reflect key points and make a complicated case easier to understand. This “example” is directly from a complaint filed by an insurance company, therefore, I am using the facts THEY presented. There are always two sides to a story so please understand this is just one side of the story. This information was found through records available to the public.