Predetermined Treatment Protocol
What Is A Predetermined Treatment Protocol?
Based upon a legitimate examination and diagnosis, a licensed medical professional must engage in medical decision-making to design a legitimate treatment plan that is tailored to the unique circumstances and needs of each patient based on several factors such as the severity of the injury, medical history, age of the patient, mechanism of injury, physical condition of the patient, and other factors. During the course of treatment, licensed medical professionals should modify treatment plans based upon the unique progress, or lack thereof, of the individual patients.
Treatment plans should be periodically reassessed and modified based upon the progress of the patient, or lack thereof.
Treatment plans for patients with soft tissue injuries such as strains and sprains may involve no treatment at all; medication to reduce inflammation or relieve pain; passive therapy; active therapy; injections; and sometimes surgery.
Passive therapy does not require any affirmative effort or movement by patients and include (a) hot/cold packs, (b) ultrasound, (c) electrical stimulation, (d) manual therapy, (e) massage, (f) manual traction, (g) mechanical traction. Passive therapy should generally be used only to the extent necessary to reduce pain and facilitate active modalities. To the extent needed, passive modalities should be administered early in treatment and transition over time to active treatments.
Active therapy requires affirmative movement by patients and includes a variety of exercises, strengthening, and stretching tailored to the unique circumstances of each patient, including the nature and location of the injuries, the patient’s’ physical abilities, and the patients’ response (or lack thereof) to any particular active therapy on any day or over time. Active modalities should generally be introduced as soon as practicable to promote the actual healing of strains and sprains.
The decision of which types of therapy are appropriate for each patient, as well as the level, frequency, and duration, should vary depending on the unique circumstances of each patient, including (a) the patient’s age, social, family, and medical history; (b) the patient’s physical condition, limitations, and abilities; (c) the location, nature, and severity of the patient’s injury and symptoms; and (d) the patient’s response to treatment.
While multiple passive therapies may be medically necessary to reduce pain and facilitate the patient’s ability to perform active therapy, the combination of five or more modalities on nearly every visit would rarely, if ever, be appropriate for any patient.
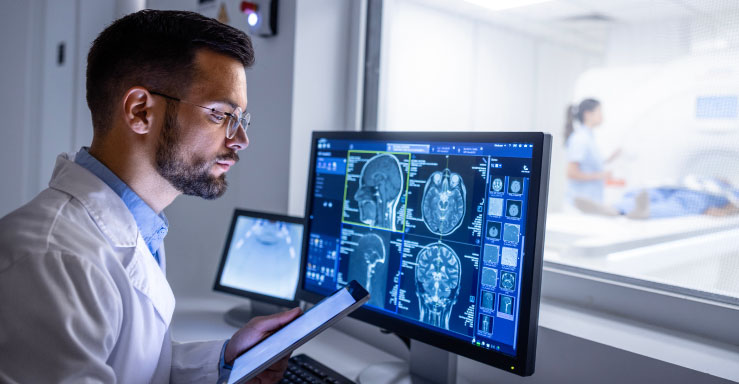
To the extent diagnostic tests such as x-rays, CTs, and MRIs are medically necessary and are performed, treatment plans should integrate their results. Patients should be discharged from treatment when they have reached maximum medical improvement, such that no further treatment is likely to benefit the patient, or when patients fail to respond to the treatment plan. MRIs are advanced imaging procedures that should be ordered if they are necessary for a diagnostic purpose to guide treatment, or another specific purpose designed to benefit the patient as explained in the medical record. For example, MRIs may be appropriate when a patient’s diagnostic picture includes worrisome signs or symptoms, response to treatment is atypical, or legitimate concerns about structural issues exist. The need for MRIs are rarely indicated on a patient’s first date of treatment. When MRIs are clinically indicated and ordered, medical providers should evaluate and document whether any abnormalities have any clinical significance for the patient’s current condition and care plan.
Patients should be discharged from treatment when they have reached maximum medical improvement (“MMI”), such that no further treatment is likely to benefit the patient with the option to return on a “PRN” or as-needed basis or when patients fail to respond to the treatment plan.
A predetermined treatment protocol is designed to financially enrich the medical providers and maximize profits; not to benefit the patients who are receiving care or to address each patient’s unique circumstances.
Common Examples of Predetermined Treatment Protocols
The most common examples would be a patient being told that they have to treat for “30 visits.” While most doctors who treat auto accident patients may agree that most people need at least 30 visits to feel better after a car crash, what happens if a patient feels miraculously better after 5 visits? Do they still need to treat for the remaining 25 visits? Does every patient that treats with that doctor need 30 visits exactly?
Other common predetermined treatment protocols include:
- A script for MRI is written for almost every patient on the X visit regardless of their pain level, body parts that they complained about, or symptoms.
- A script for DME is written for almost every patient on the X visit
- Every patient is told to treat X times for the first week; X times per week for the next four weeks; and X times for the next four weeks.
- Patients in an accident on the same day getting discharged on the same day (even if they were all on the same accident)
This “one size fits all” approach doesn’t have to be for “every patient” either. This can be for “almost every patient” and even a “majority of patients.” Remember that each patient should receive individualized care tailored to the unique circumstances and needs of their situation based on several factors such as the severity of the injury, medical history, age of the patient, mechanism of injury, physical condition of the patient, and other factors.


